Life After Spinal Fusion Surgery:
A Month-By-Month Breakdown of My Spinal Fusion Recovery
I get a lot of messages from people who’ve had spinal fusion surgery. Many are in the first few months of their recovery. Most ask some variation of the question, “is my recovery normal?”
“I’m 6 weeks post-op and tire after 15 minutes of walking. Is that normal?”
“I’m 12 weeks post-op and my surgeon lifted all of my restrictions already. Is that normal?”
“I’m 4 months post-op and I’m still exhausted all the time. Is that normal?”
The answer in my head is always the same: “I have no idea.”
Because honestly, I don’t even know if my own surgery recovery was/is normal. Was it quicker or slower than average? Did I have more or less pain than normal? Did I take pain meds for too long? Or for not long enough?
The answer to all of the above is yes. Because there is no normal. Each one of us will experience spinal fusion surgery differently.
“Hope is not about proving anything. It’s about choosing to believe this one thing, that love is bigger than any grim, bleak shit anyone can throw at us.” – Anne Lamott
I totally understand the need to compare notes though. I do it too. What choice do we have? There’s no guidebook with an estimated timeline for your recovery – a “What to Expect When Your Bones are Fusing,” if you will. And even if you have the most attentive & compassionate surgical team in the world, they don’t want you calling their office every day with questions about weird symptoms or your poop. Neither does your pharmacist or your physical therapist.
We all just want some sort of benchmark – something to reassure is that we are, in fact, normal. And more importantly, that things will get better.
I don’t know if I’m normal or not, but as always I’m happy to share my experience with you. I’ll break it down for you as much as I can, to the best of my recollection (some of it is a little hazy). Then let’s compare notes. Share your own experience for others who might need to hear it. (Note: I’m including some of my blog and Instagram posts from those first few months to help me paint a clearer picture for you.)
What to Expect After Spinal Fusion Surgery
Recovery from Spinal Surgery: Week 1
My surgery was on a Thursday morning. I spent two nights in the hospital. I had some visitors and my husband was with me the whole time, but I think mostly I just slept a lot.

I was sent home with a cold therapy machine and prescriptions for Robaxin and Oxycodone. My insurance company provided a walker, and we borrowed a shower chair (an absolute essential for at-home recovery).
“oh, my darling, it’s true. Beautiful things have dents and scratches too.” – @writtenbyhim
On the way home from the hospital, we stopped at the pharmacy to pick up my prescriptions. I wasn’t able to walk, so Vic pushed me in a wheelchair. When we got home, I somehow managed to walk through the front door, hobble up the stairs, and heave myself into bed, where I would stay for most of the next 10 days.
I only got out of bed to use the bathroom, take a shower, or when my physical therapist made me. Getting in and out of bed was brutal. I was in a lot of pain. Way more than I expected. I spent most of that first week sleeping and counting the minutes until my next dose of pain meds.
Week 1 at a Glance:
- I could get to and from the bathroom myself with the help of my walker.
- I needed help with just about everything else, including getting in and out of the shower and dressing myself.
- The only exercise I got was in-home physical therapy twice a week.
Recovery from Spinal Surgery: Week 2
During the first two weeks, I had terrible, scary nerve pain in my left leg. This was particularly frightening because my pre-op pain was almost entirely in my right leg and hip. But my surgeon reassured me with some statistics (that he probably made up, now that I think about it) about leg pain being common after a spinal fusion.
I relied less on the walker, but I still spent most of my time in bed, only occasionally getting up to shuffle around my bedroom.
Week 2 at a Glance:
- I could walk around the house without a walker.
- I could walk up & down the stairs.
- I was able to shave my legs.
- I was sleeping fairly well at night, usually only waking when I needed pain meds.
I wrote this blog post at day 13 of my spinal fusion recovery – it goes into greater detail about my experience.
Recovery from Spinal Surgery: Week 3
The nerve pain wasn’t gone by week 3, but it was more manageable. That’s when I really started to notice the discomfort in my back. Not pain, exactly. More like I had a brick strapped to my lower back. In a way, this was scarier than the leg pain – I was convinced that this was my hardware poking through my skin and that my back would feel this way forever. (Spoiler: it didn’t.)
I had my first post-surgery outing – dinner at The Loop with my husband.

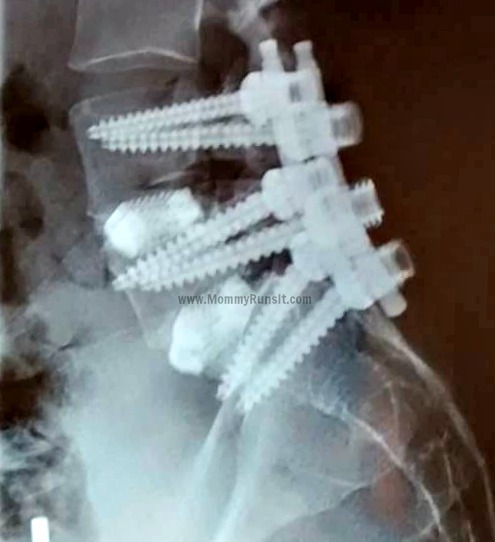
I also had my first follow-up visit with my surgeon during week 3, and I had my first set of post-op x-rays. Vic and I were stunned to see the size of the screws in my back.
My incision site was red and itchy, but it turned out to be an allergic reaction to the bandage adhesive. I was healing well and moving around the house with more ease, but I continued to spend the majority of time in bed – largely because lying on my back with my legs propped up on pillows was the most comfortable position for me to be in. Sitting upright was uncomfortable, and I could only stand for short periods at a time.
This week was also my last week of full-time recovery. Vic was back at work, but my kids were at overnight camp. I didn’t have much to do besides resting and healing.
Week 3 at a Glance:
- I no longer needed the walker. I walked slowly, but I was steady on my feet.
- I was able to do small household tasks, like folding laundry and making a grilled cheese sandwich.
- I was still taking pain meds throughout the day but had started weaning myself off the Oxycodone.
- I was able to tolerate short car rides.
Recovery from Spinal Surgery: Week 4
By week 4, I was officially back on full-time Mom Duty, at least during the day. I still needed Vic to do a lot around the house – cooking dinner, bath time, making our morning coffee. He also took over the grocery shopping, which he continued to do up until fairly recently. (Even now, it can still be hard for me to carry the groceries and be on my feet for that long. Plus I just like having him do it. Not gonna lie.)
I was able to drive short distances, which also meant that I was able to go without pain meds during the day.
By the end of the day, I was usually in a fair amount of pain, which meant pain medication and back to bed with ice on my back. I don’t recall if I was still having leg pain at this point, but if I was it must not have been too bad. Most of the pain was in my back at the fusion site. Some of the swelling had subsided, but the feeling of having a brick in my back wasn’t completely gone.
And speaking of bed – yes, that’s where I was still spending a lot of my time. We moved a TV into the bedroom, so the girls spent a lot of time laying with me and watching Netflix. We don’t normally have televisions in any of our bedrooms, so this was a treat for them. And they also enjoyed the temporary lift of the “no eating in bed” rule. After spending much of the past few weeks alone, I enjoyed their company very much.
Week 4 at a Glance:
- I was able to drive for short distances.
- I was mostly weaned off of daytime pain meds, but I still took them in the evenings and before bed.
- I didn’t do any intentional exercise – just relied on caring for the kids and walking up & down the stairs 100 times a day to keep active.
- I tired very easily and napped daily.
Recovery from Spinal Surgery: Weeks 5-6
By weeks 5 and 6, I started feeling a little anxious/guilty about the slow pace of my recovery. I’d expected to feel nearly recovered by then, which wasn’t even remotely the case. I was still slow and stiff and tired all the time. I was back on my feet, though. Life was normal-ish. I took the kids to the pool and out on little errands, and I was even brave enough to take Sophia (just the two of us) to the beach for a few hours.
At my 6 week follow-up visit, my surgeon cleared me to practice very gentle yoga, but I didn’t feel at all ready. I was very worried about re-injuring myself. I walked when I could, but I still wasn’t doing any real exercise, including my physical therapy exercises (I wish I’d been more diligent about them).
Weeks 5-6 at a Glance:
- My pain was manageable; most of the time I felt stiffness and/or discomfort, rather than actual pain.
- I was only taking pain medication at night, so my head was clearer.
- Still tired, still taking daily naps.
Recovery from Spinal Surgery: Weeks 7-8
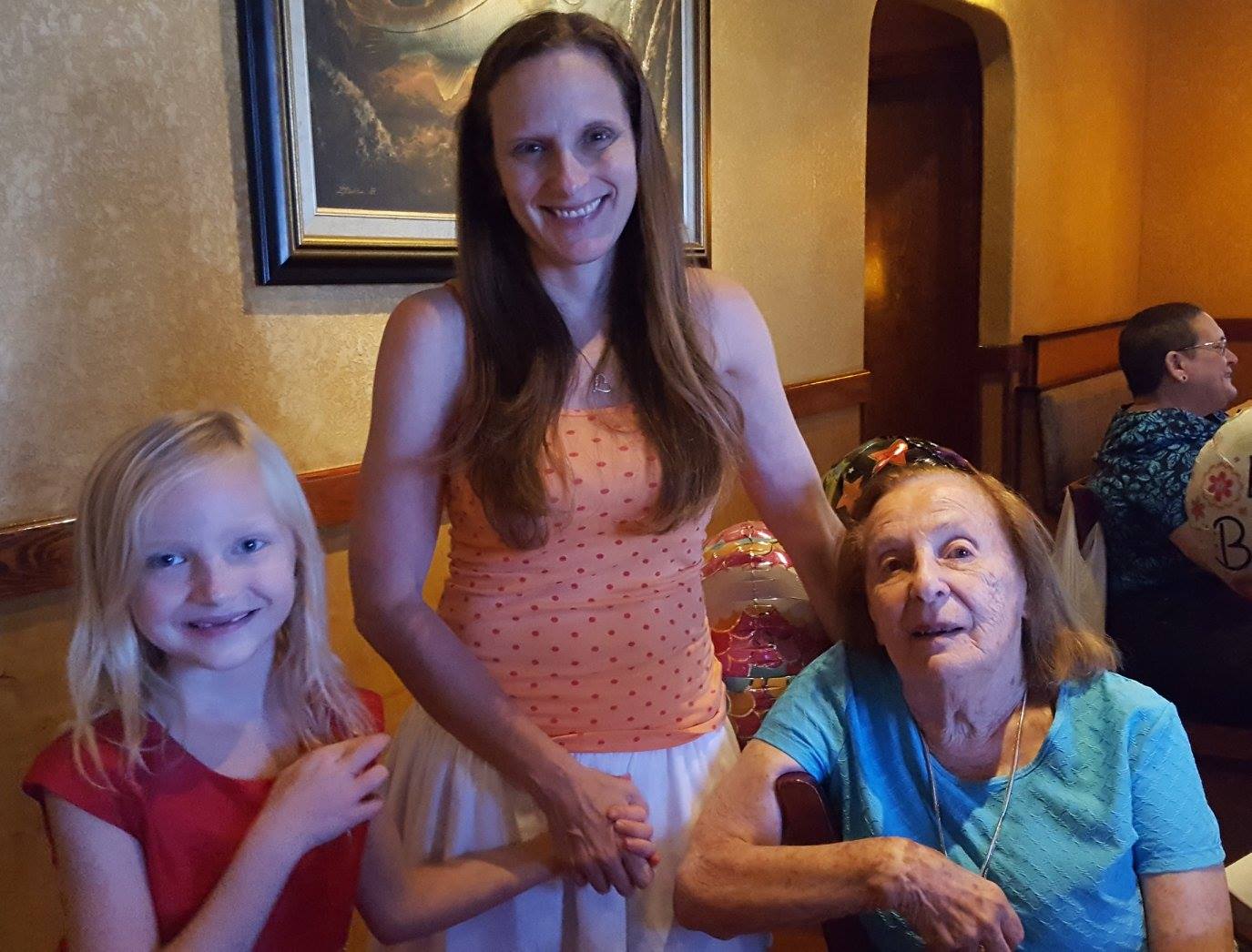
During week 7, I went on my first post-op road trip for my grandma’s 95th birthday party. It was about a 4 hour drive, and while it wasn’t the most comfortable experience of my life, it wasn’t too bad.
I pushed myself a little too hard on this trip though, and I ended up with some weird symptoms – muscle spasms, headache, etc. And, of course, I was exhausted like always.
I wrote a blog post describing life at 8 weeks after spine surgery, and it describes things much better than I could now. It’s called, fittingly, “Not Normal Is the New Normal.”
Recovery from Spinal Surgery: Weeks 9-12
I’ll just hit the highlights here.
Week 9: I finally started practicing some very gentle yoga and stretching.
Week 10: I went kayaking with my family for the first time ever, and I didn’t experience any pain!
Week 11: The kids went back to school, and I took this picture in my driveway. (I don’t advise jumping at 11 weeks post-op – it hurt afterwards.)
Week 12: I started a regular walking routine, usually solo morning beach walks, but sometimes with a friend.
Life After Spinal Fusion: 3 Months
I drove myself to my 3 month follow-up appointment with my surgeon. I had x-rays taken, and he said that everything looked great. I asked if he could see any evidence of bone growth, and he told me that it was too soon for it to show up on an x-ray. He lifted all of my restrictions – not just BLT (bend, lift, twist), but ALL of them – he essentially said that I could do whatever I wanted, as long it didn’t hurt. The only things he specifically told me to avoid were sit-ups, crunches, and push-ups. Everything else was fair game.
He also said that I was free to start running and yoga again, but that I should avoid any activity that caused pain. He stressed that there was no benefit for me to “push through the pain,” as pain (not muscle strain or discomfort) was an indication that something was not right.
And then he released me from his care, which I was not expecting at all. No 6 month follow-up, no annual check-ups – just good luck, and call us if you have any problems.
Life After Spinal Fusion: 4 Months
Early in my 4th month of recovery, we took a family vacation to Washington, D.C. It involved a lot of walking, and I came back to the hotel and crashed every day around 5:00 p.m. But other than that, the trip was a great success.

In the first year after my surgery, we also visited Disney World (7 months post-op), Colorado (9 months post-op), and New York (12 months post-op). I also took a solo trip to Colorado at 11 months post-op.
At the 4 month mark, I was feeling relatively normal – still a bit slower and stiffer than usual, and certainly not back to my pre-injury level of physical activity, but definitely a lot more like myself. The only major symptom that I was still experiencing at that time was exhaustion. Constant, almost oppressive exhaustion. I still required daily naps in order to make it to bedtime. But on the bright side, I usually only need to sleep for an hour or so, whereas I was napping for 2-3 hours at a time in previous months.
By this time, I’d stopped taking pain meds almost entirely. I occasionally needed a pill at bedtime when I’d overdone it during the day, but that was it.
Life After Spinal Fusion: 5 Months
This blog post describes pretty thoroughly what my life was like at 5 months after my spine surgery.

Life After Spinal Fusion: Your Turn!
There you have it – my first 5 month of recovery in a nutshell. If you want to know more details about any phase of recovery, or if you have any questions (general, specific, personal, weird, whatever) please ask me! I want to help you as much as I can. Also – if you’ve had spinal fusion surgery, please chime in here. I don’t want this to be just about my experience. I want to hear yours too, and so do others, trust me.
For more recent updates on my post-op life, read these posts:
One Year Post-Op: Spinal Fusion Update: One Year Later (A Letter to Myself)
Three Years Post-Op: Life After Spinal Fusion: I Went Skiing at 3 Years Post-Op!
Five Years Post-Op: Five Years After My Spinal Fusion: An Update
